Science | Sport | Policy | Perspective
First published as a newspaper column in 1999, this journal shares personal perspectives, research, humor and insights from clinicians, caregivers, parents, teens, schools, coaches, and healthcare leaders seeking positive changes in access, treatment, and outcomes.
Search the archive:
Addiction
San Francisco Goes Against Tide To Help Homeless Facing Addiction
Addiction Recovery Model Uses Craving & Anxiety Scales To Reduce Relapse Risk
Aging
Parents: New, Old & Overwhelmed
Moms Rely On OBGYNs, Dads On Urgent Care, Neither On Insurance
200,000+ Follow Addiction Social Media Sites, But Parents Could Use Better Direction
Managed Care
Coronavirus Impact Study Reveals Anxiety Levels Rising, But Tele Response Escalating
California Health Plan Provides Support To PCPs On Mental Health
Insurer Program Attempts to Integrate Medical & Behavioral Data
Docs & Hackers Meet-Talk About Mental Health, Diabetes ‘Apps’
Patients Getting Physical Therapy Who Really Need Psych Services
Adolescence
Autism
Sports & Leisure
Mood Monitor
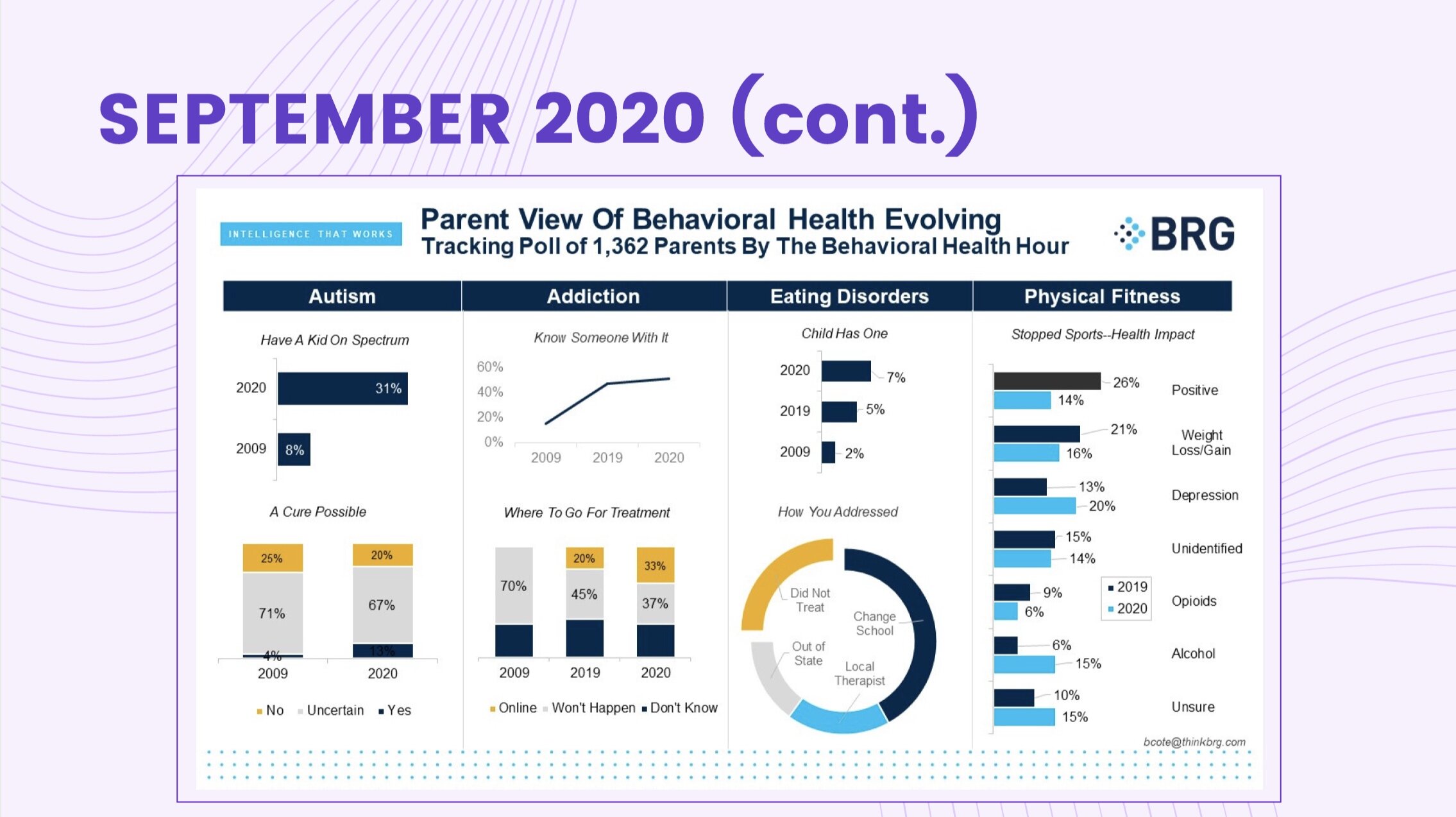
A snapshot of the country’s emotions, attitudes and mental health
Swipe through the latest below